Have you ever done an elimination diet or removed the big food triggers like gluten or dairy to improve your Crohn’s disease or ulcerative colitis symptoms? Have you ever felt disappointed that it didn’t make as big of a difference as you expected? Maybe it gave temporary relief, but your symptoms persisted.
I see this quite often.
Fortunately, there is a reason. Let’s dive in.
The first step in healing the gut
When it comes to healing the gut, food eliminations are an important step. You cannot heal if you’re repeatedly eating foods that are leading to inflammation or persistence of your symptoms. Therefore, it’s imperative that any trigger food (or potential trigger food) is removed for an extended amount of time.
This stops the “insult to injury” cycle in terms of diet, at least.
This is step 1.
If you stop here you will likely feel frustrated that this didn’t fix all your problems.
But removing trigger foods doesn’t fully heal the inflammation, gut permeability, or microbiome imbalance that remains (but it does help).
Add in gut-loving, anti-inflammatory foods
After removing the trigger foods, your gut is depending upon you to put the right foods in!
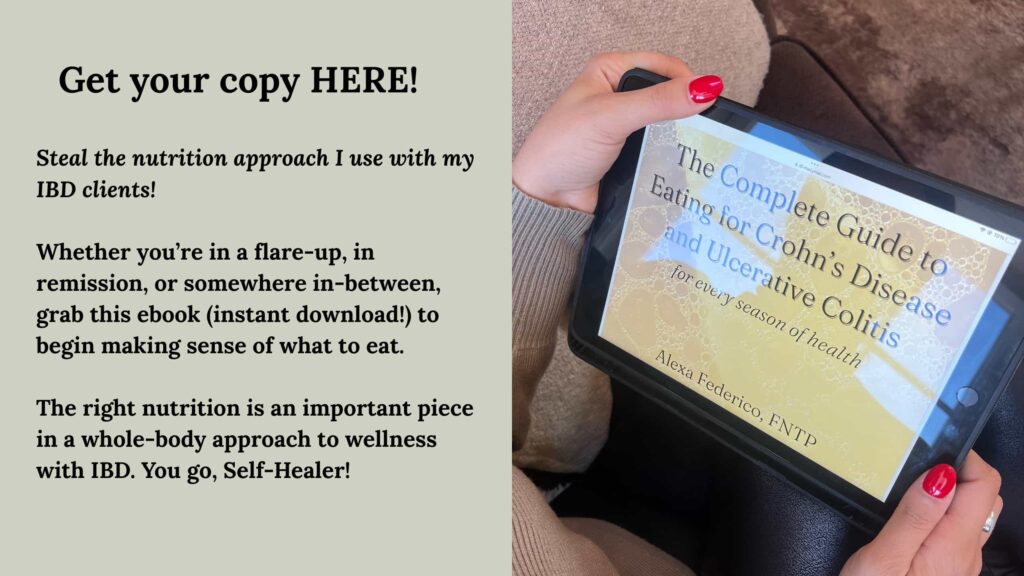
For a full run down of what I recommend to eat for IBD, whether you’re in a flare, in remission, or somewhere in-between, grab my ebook, The Complete Guide to Eating for Crohn’s Disease & Ulcerative Colitis.
At a high level, the focus is on whole foods.
Think foods grown in the ground, caught in the ocean, or raised on a farm.
This covers our meats, eggs, seafoods, veggies, fruits, nuts/seeds, properly sourced oils/fats, some grains, dairy. All as tolerated of course, but this is what makes a superfood, anti-inflammatory diet. These foods (when tolerated) are naturally health-promotive and anti-inflammatory.
When you’re healing from a flare, or are in a season with a lot of food intolerances, warm and well-cooked foods are the priority, Think soups, stews, bone broth, beef roasts, and soft veggies, Keep it simple.
Supplemental support
So now, you’ve removed trigger foods. You’ve added in whole foods your body will love.
Awesome.
Let’s take it a step further.
Including the right types of supplements can truly expedite the IBD healing process. The two forms of supplements to use first are herb/plant formulas (calm inflammation, heal the tissue), and supplements that help the functionality of digestion (enzymes, bitters, HCl, and for some liver/gallbladder supports). These ingredients are concentrated in the supplement meaning, you’re packing a healing punch in that tincture, powder, or capsule.
In my Fullscript store where my recommended supplements are, these are currently labeled on protocols called, “Healing the Gut.” There are many herbs that are effective. A few are curcumin, aloe vera, slippery elm, marshmallow, zinc, and more. My recommendations for the digestive aids is labeled as such on Fullscript. I wrote a blog post on my favorite supplements for IBD where you can find more explanation on these.
And then there are probiotics; necessary gut bacteria that populate the large intestine that are needed for normal bowel movements, keep the immune system strong, heal the gut lining, and more. Foods like fermented foods (sauerkraut, kefir, yogurt, kimchi, kombucha, etc.) have naturally-occurring probiotics, while different fruits, veggies, and grains have prebiotics that feed the probiotics. When tolerated, these are functional foods, meaning they are multi-purposeful in addition to their basic nutrients. I still recommend taking a probiotic for IBD healing (my recommended is on Fullscript).
Including medicinal powerhouses like these supplements are another common missing puzzle piece to many people’s IBD healing plan. Once my clients introduce these, they often see improvements in how they feel.
Lifestyle factors
The many lifestyle factors (sleep, stress, movement, mindset, daily habits, etc.) certainly impact digestion and overall health. I work with my clients to optimize these as well. Gut health truly takes a whole-body/whole-life approach. I won’t go into specifics for each of these lifestyle factors in this article, but know they are very important to address on the gut-healing journey.
The takeaway
Removing gluten is not a waste just because it didn’t heal you.
The fact that you have more food intolerances after an elimination diet is not the elimination diet’s fault.
These situations result from a gut-healing protocol that is missing some key steps!
For step-by-step support
Sign up for one-month of personalized nutrition, lifestyle, and chronic illness mindset support with me. Let’s lay the groundwork for healing!
Or, grab the ebook that hundreds of IBD Self-Healers have used to make eating for IBD less confusing!