What is CBD?
CBD is an acronym for cannabidiol and is one of the many different chemicals found inside Cannabis sativa, and it has been showing very promising results for pain and inflammation. The species Cannabis sativa includes both plants known as marijuana and hemp. These are the common names for two different “chemotypes” or “chemovars.” These are different strains of the same plant species that have been bred to produce a specific mixture of chemicals. For example, Marijuana was bred to produce more cannabinoids like THC (Tetrahydrocannabinol), whereas hemp was bred for fiber production and now CBD production.
Most CBD bought and sold comes from hemp due to legal restrictions on marijuana and the separate market for THC. Laws for Cannabis sativa and cannabinoids vary greatly between localities. Always check local laws if you are uncertain about the legal status and restrictions in place. Supplemental use is widely acceptable and should not pose any issues for most people.

Why do People use CBD for Pain?
There is currently a huge demand for CBD containing supplements. Many companies offer an extensive variety of CBD products online and in-store. Amongst CBD users, about 62% have reported using it to treat a medical condition (Corroon, 2018). Studies have shown the potential of cannabinoids to treat many different medical conditions and CBD is no exception. Surveyed CBD users reported pain, anxiety, and depression as the most common reasons for their CBD use, and almost 36% of respondents said it treated their condition very well by itself (Corroon, 2018).
Aside from the perceived effectiveness of CBD for treating pain, it also seems safe in most users. The intoxicating effects of other cannabinoids like THC are not an issue and CBD does not cause addictions like opiate pain medications. On the contrary, CBD has shown promise in treating addictions to alcohol, nicotine, cocaine, and opiates (Weiss, 2018). The promising potential of CBD, limited options for treating pain, and side effects of other treatments has peaked interest in it.
How Does CBD Alleviate Pain?
CBD affects how your nerves send pain signals and how your brain interprets them. How the pain signal is sent is called nociception, how our brain reacts to those signals is called pain perception. Pain can also be caused by damaged or malfunctioning parts of the brain, spinal cord, or nerves. Pain originating from the brain, spinal cord, or nerves is called neuropathic pain. This type of pain is difficult to treat and often chronic. Fortunately CBD has a positive effect on some types of neuropathic pain by regulating nociception and pain perception. CBD is also very effective at stopping inflammation.
Why does Inflammation Matter?
By lowering inflammation CBD can actually help lower pain levels. When your body senses damage caused by a physical injury, infection, toxic substances, etc. it sends signals to specialized cells to cause inflammation. These inflammatory cells are part of the immune system. They use inflammation to remove whatever is causing the damage and the damaged cells before starting the healing process. As inflammation occurs the affected area becomes swollen, turns red, loses it’s function, and feels warm and painful. Because inflammation causes pain, treating the inflammation can be very effective in stopping the pain. Eliminating inflammation is how anti-inflammatory drugs help relieve pain. Common examples of these anti-inflammatory pain relievers are acetaminophen and ibuprofen. Acetaminophen relieves pain and inflammation through the endocannabinoid system but in a different way than CBD does (Klinger-Gratz, 2018).
What Mechanisms are Involved in Your Body?
The details of how CBD works to relieve pain and inflammation are extensive and we do not currently understand them all. Nonetheless, through research we have learned a lot of the mechanisms, and some will be further explored to create new drugs even better than current treatments. Below is a list of the known mechanisms:
- Cannabinoid Receptor 1 (CB1) – This type of receptor is located in the brain, spine, and nerves. The CB1 receptors influence the process of nociception by changing how sensitive nerves are to sending signals (Palazzo, 2010). CBD is considered a negative allosteric modulator of the CB1 receptors (Laprairie, 2015). This means it weakens the effects caused by other cannabinoids acting on CB1. By changing how the cannabinoids (made in our body and from our diet) affect these CB1 receptors CBD changes how we feel pain (Alaverdashvili, 2018; Manzanares, 2006). The CB1 receptors can also connect to other receptors such as opioid receptors in a process called dimerization. These dimers change how the opioid receptors work and change how we feel pain (Bushlin, 2012).
- Opioid receptors – There are three opioid receptors: Kappa, Mu, and Delta. The Kappa receptor helps regulate the effects of a variety of opiates. The Mu receptor is responsible for the effects from morphine, fentanyl, and codeine. Many drugs that act directly on the Kappa and Mu receptors cause intoxication and addiction. The Delta opioid receptor is involved in pain perception and our emotional response to it, in particular our anxiety from experiencing pain (Quirion, 2020). This makes the Delta opioid receptor very important for chronic pain due to the addiction issues with the other receptors. Mu and Delta opioid receptors are both influenced by CBD through dimerization with the CB1 receptors mentioned above (Bushlin, 2012). There are less intoxicating and addictive side effects by indirectly acting on the Mu and Delta opioid receptors to treat pain. This is why CBD is not addictive despite effecting the Mu opioid receptor indirectly.
- Cannabinoid Receptor 2 (CB2) – The CB2 receptors are located throughout the body and are mostly located on the tissues involved with the immune system. These include the spleen, colon, tonsils, lymph nodes, and white blood cells. These receptors modulate metabolism, body fat, inflammation, and the immune system. CBD is capable of activating the CB2 receptors (Tham, 2018). Through the CB2 receptors CBD lowers inflammatory pain by reducing the amount of inflammatory cytokines and T-cells in your body (Atalay, 2019; Jean-Gilles, 2015; Petrosino, 2018). However, the CB2 receptors were found to not be effective in treating acute pain in several studies (Bie, 2018). This suggests that CB2 receptors are useful for chronic inflammatory or neuropathic pain but not nociceptive pain from injuries.
- G-Protein Coupled Receptor 55 (GPR55) – GPR55 is somewhat similar to CB1 and CB2 receptors and has been contested as a possible CB3 receptor. However, categorization is difficult and is still controversial. Regardless, GPR55 has been implicated in modulating inflammatory and neuropathic pain in animal studies (Staton, 2008). For example, inhibitors of the GPR55 receptor have lowered intestinal inflammation in separate animal studies (Stančić, 2015). Reducing intestinal inflammation reduces the inflammatory pain associated with it. CBD is an inhibitor of the GPR55 receptors (Godlewski, 2009) and therefore may lower inflammation and pain by blocking the receptors. This still needs to be confirmed with CBD, but most evidence suggests blocking GPR55 does lower nociception (Deliu, 2015).
- 5-Hydroxytryptophan Receptors (5-HT’s) – This is the chemical name for serotonin receptors. These receptors are located in the brain and peripheral nervous system like the spine and nerves. These receptors are incredibly diverse and regulate the transmission of many different neurotransmitters. Through regulation of these neurotransmitters the serotonin receptors affect mood, movement, appetite, sleep, memory, and pain. The serotonin receptors (5-HT’s) are classified into 7 different groups, 5-HT1 to 5-HT7. Each group has different subtypes specified by a letter. For example 5-HT1A or 5-HT2C. Pain, especially chronic pain, can destabilize serotonin receptors and this can cause anxiety, depression, and aggression.
Essentially, serotonin receptors are involved in your pain perception. CBD is known to bind to the 5-HT1A and might also bind to the 5-HT2A receptors to a lesser extent (Russo, 2005). CBD has shown beneficial effects on pain perception through serotonin receptor modulation in animal studies (Gregorio, 2019; Jesus, 2018; Ward, 2014). In a study on human Blood Brain Barrier (BBB) cells CBD also had an effect on 5-HT1A receptors (Hind, 2015). More research is needed to understand CBD in humans but the current research is predictive that CBD is useful for the treatment of pain perception.
- Adenosine A2A Receptor (ADORA2A) – There are four types of adenosine receptors in your body. The A2A receptor is involved in regulating the cardiovascular system and inflammation. It also has an effect on the neurotransmitters glutamate and dopamine. This can change how you feel pain and how awake you feel. For example, caffeine acts on the adenosine receptors to produce wakefulness. Chocolate, tea, and coffee are all used to stay awake by blocking the adenosine receptors. CBD activates the Adenosine A2A receptor (McPartland, 2015) which might explain some of it’s sedating effects. By activating the Adenosine A2A receptor CBD lowers inflammation (Mecha, 2013). Along with reducing inflammatory pain CBD might also be affecting our perception of pain by changing how adenosine is transported to and from the receptors. The significance of the effects on adenosine transportation to the adenosine receptors is still not definitively known (Ibeas Bih, 2015).
- Peroxisome Proliferator Activated Receptors (PPAR’s) – The peroxisome proliferator activated receptors are located inside the middle part of cells called the nucleus. This is where your DNA is located. Different factors influence the DNA to change how genes are expressed, this in turn changes how the cells function. The PPAR’s are some of the factors inside the nucleus that influence gene expression. They are mostly involved in the metabolism of fats, oils, and sugar but they also influence inflammation. Like many other classes of receptors the PPAR’s consist of a group. The different receptors are known as PPAR-alpha (PPARa), PPAR-delta (PPARd), and PPAR-gamma (PPARy).
The PPARy receptor is very important in inhibiting inflammation and inflammatory pain. PPARy stops another factor, called nuclear factor kappa-light-chain enhancer of activated B-cells (NF-kB) from causing inflammatory expressions of genes. When NF-kB is unable to cause inflammatory genes from expressing themselves, the cells are not targeted by the immune system. This can significantly help with inflammatory pain as well as other inflammatory conditions such as diabetes. CBD is capable of activating PPARy to cause these anti-inflammatory effects (Atalay, 2019; Nahler, 2018; O’Sullivan, 2016).
- Transient Receptor Potential ion Channels (TRP’s) – These receptors are involved in the process of sensing temperature, vibration, pressure, vision, and some tastes. They do this by changing how ions (particles with an electrical charge) pass through the membranes on cells. There are many of them but CBD specifically acts on TRPA1, TRPV1, TRPV2, TRPV3, and TRPV4. Aside from activating these TRP channels, CBD blocks TRPM8 (Nahler, 2018; Petrocellis, 2008). The TRPV1 receptor is responsible for some of the pain relieving and anti-inflammatory effects of CBD in animal studies (Costa, 2004). Many other studies suggest CBD desensitizes the TRPA1, TRPV1, TRPV2, TRPV3, and TRPV4 receptors to painful stimuli (Petrocellis, 2011). This is the same way capsaicin from chili peppers helps with arthritis pain.
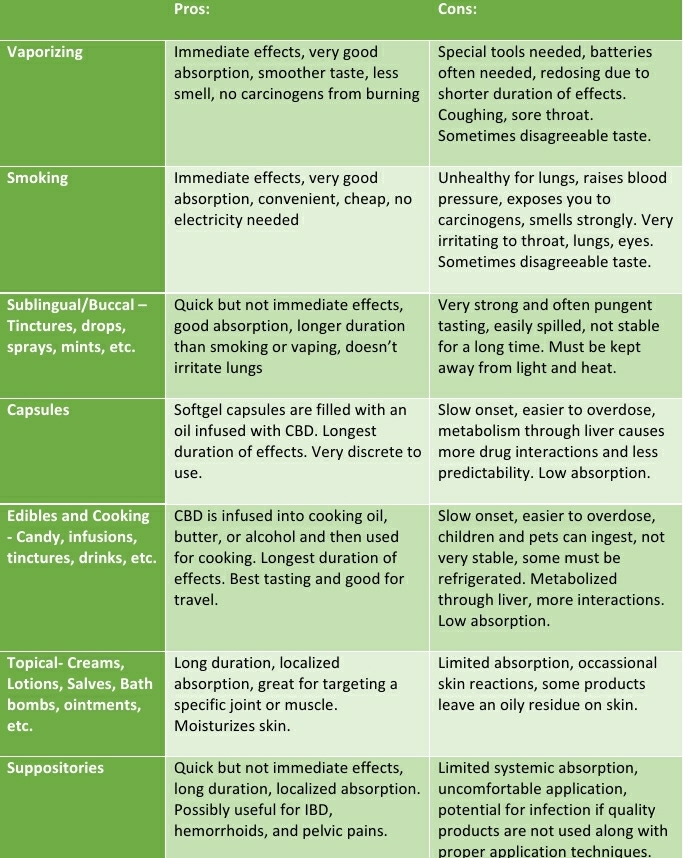
How is CBD used?
CBD can be used in a variety of different ways. Each method has pros and cons and each person must use trial and error to decide what suits their needs best. A combination of different methods is preferred by some people. For example, you might take a 50mg CBD capsule twice a day and vaporize as needed.
The Difficulty of Dosing
Dosing is still not entirely well-understood and few guidelines exist for specific illnesses, demographics, and contradictions. For example, nobody can definitively state what is an appropriate amount of CBD for a child with juvenile arthritis or an adult with social anxiety disorder and comorbid fatty liver disease. Until more studies have been done to evaluate the therapeutic window of CBD for a variety of diseases and demographics we are limited to trial and error. Along with the limitations of current studies, there are a number of factors that make recommendations difficult.
- Diet can change CBD absorption several ways. CBD dissolves in oils and fats so eating food with your dose can increase it’s effectiveness (Millar, 2018; Zgair, 2016). Certain phytochemicals found in food and spices also change how effective CBD is metabolized, these include things like piperine, curcumin, and resveratrol (Izgelov, 2020; Cherniakov, 2017).
- Body Fat is closely connected to the endocannabinoid system. How much body fat you have and how it is distributed on your body can change how much CBD you need (Fattore, 2010; Huestis, 2007). The effects might also last longer or feel differently if you are gaining or losing fat. This is because many cannabinoids dissolve in fats and oils, including those in your body. Other cannabinoids like THC have been shown in animal studies to be stored in fat cells. When the fat is burned it releases the stored THC back into the blood (Gunasekaran, 2009).
- Sex and Hormones also influence how your body reacts to CBD. Differences between men and women and the relationship between cannabinoids and the endocrine system are still lacking but some animal studies have shown interesting patterns. Sexual brain differences and testosterone and estrogen levels seem to be very important factors (Craft, 2013). The pain relieving effects of THC are increased in female rats during estrous due to higher estrogen levels (Craft, 2008). Whether this also applies to CBD is unknown at this time. Women also seem to absorb CBD better (Iffland, 2017). Human studies are needed to better understand the complex interaction between hormones, sex, and cannabinoids.
- Age makes a difference in how you respond to CBD just like it does for other drugs. You should talk to a doctor or pharmacist if using CBD as a child or elderly person. They can help you decide which CBD-containing products and at what doses are most appropriate. Children and the elderly have special needs due to differences in how their bodies process drugs, supplements, and food.
- Drugs and Supplements are also likely to affect how CBD is absorbed and how it works in your body. There are too many interactions to list, so it’s best to consult a pharmacist or doctor if you plan on taking other drugs or supplements with CBD.
As you can see there are many factors that affect dosing. It might seem daunting to decide what dose to start with, but there are several easy guidelines to make things as safe as possible. These are very generalized tips for dosing with any new supplement:
- Talk to your doctor before starting so they can check for interactions and offer any advice they might have specific to your medical history and current treatment.
- Start with smaller doses before trying larger amounts. Build up to an average sized dose and make adjustments as needed. You might need more or less as your condition(s) improves or worsens.
- Follow any provided directions and discontinue use if you experience side effects. Most supplements will come with instructions regarding how-to and how much of the product to use.
- Call 911 or go to the nearest emergency room if you experience symptoms of severe allergic reaction and anaphylaxis including: difficulty breathing, swelling of the throat, tongue, or face, rash and hives, fainting, etc.
What are Some Common Doses?
The most studied methods of use are oral and sublingual/buccal. A review of 35 studies, showed oral and sublingual/buccal doses of 1-50mg/kg/day were well tolerated and used to treat schizophrenia, SAD, epilepsy, cannabis dependency and graft‐vs‐host disease (Millar, 2019). This table shows some of the doses converted to pounds as an example of the sublingual/buccal and oral doses that have shown therapeutic effects without major side effects:
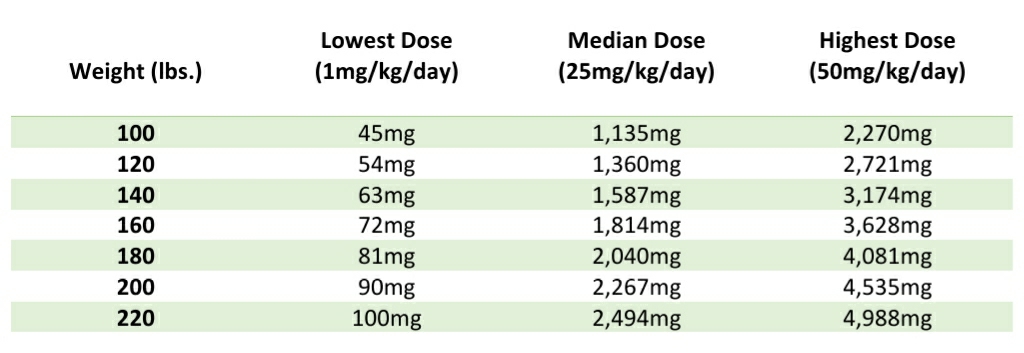
There are not as many studies on the other methods of use but topically applied CBD can be used as much as needed without side effects other than mild skin irritation and allergic reactions if your skin is sensitive. Animal studies have shown doses between 0.6mg/day to 62.3mg/day to be effective in helping arthritis pain and inflammation without noticeable side effects (Hammell, 2016). A study on peripheral neuropathy in humans also showed benefits without noticeable side effects using a product with 250mg/3floz. (Xu, 2020). Commercial products as concentrated as 1,125mg/3floz can be found for sale and seem to be well tolerated.
Suppositories’ dosages are normally in the range of 10mg to 100mg. This is the least studied method of using CBD. It is relatively new and there is some debate about their effectiveness.
Inhalation methods like vaporizing and smoking are the most effective ways to absorb CBD when the inhales are held in for a long time. These methods allow very high doses of CBD with immediate effects but a very short duration.
Some studies have been done on how well your body absorbs CBD using the different methods. This can give you a very simple comparison of inhalation doses vs. Oral and Sublingual/Buccal doses. Assuming the absorption of oral/sublingual/buccal is 5-30% (average 18.5%) and inhalation is 10-60% (average 35%) you can see that inhalation roughly doubles the amount absorbed (Bruni, 2018; Meyer, 2018)
Inhalation also increases how much CBD is absorbed at once, this causes a higher peak concentration in the body. Inhalation in one study caused a peak concentration of 7ng/ml with a dose of 0.696mg which equals about 10ng/ml/mg (Meyer, 2018) In another study 700mg orally caused a peak concentration of 10ng/ml or about 0.014ng/ml/mg (Consroe, 1991). That’s about a 700x difference in the peak concentrations between equivalent doses taken orally and inhaled! These are extremely rough estimations but nonetheless they show significant differences between the two methods:

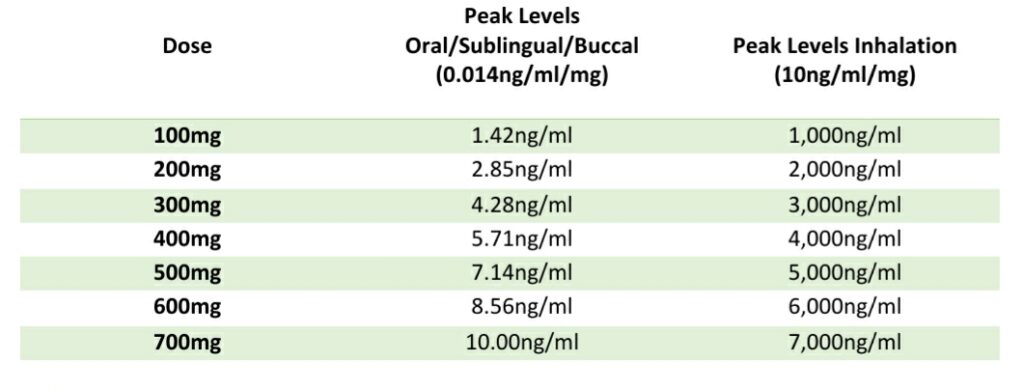
The increased absorption of inhaled CBD and the peak concentrations achievable can possibly lead to different effects with larger or more frequent doses. For example CBD has been shown to inhibit the Breast Cancer Resistance Protein 1 (BCRP/ABCG2) in what would be considered a large dose, estimated at about 2,100mg+ oral CBD or 26.67ng/ml (Iffland, 2017; Holland, 2007). Using the estimates above it would only take approximately 8mg of inhaled CBD to reach this level (26.67ng/ml ÷ 10ng/ml/mg = 2.667mg x 35% = 8mg).
This is important because BCRP/ABCG2 can change how much your body absorbs other drugs such as breast cancer treatments, sulfasalazine for IBD, and cimetidine for stomach acidity. Normal oral doses do not lead to the levels needed to do this but vaping and smoking possibly could, especially in chronic or heavy users. For the average user who is not inhaling CBD these types of effects are not likely unless dosing thousands of milligrams a day.
What are the Known Side Effects?
The limited studies available have shown CBD to be relatively well tolerated with few to no major side effects being reported (Bergamaschi, 2011; Millar, 2019; Manini, 2015). Nonetheless there are a few side effects to be aware of and some drugs that should be used with caution while used with CBD (Iffland, 2017). Here is a list of the more common side effects experienced:
- Decreased Appetite and weight loss
- Difficulty falling asleep
- Weakness, fatigue, clumsiness
- Rash
- Diarrhea
- Increased risk of Infections
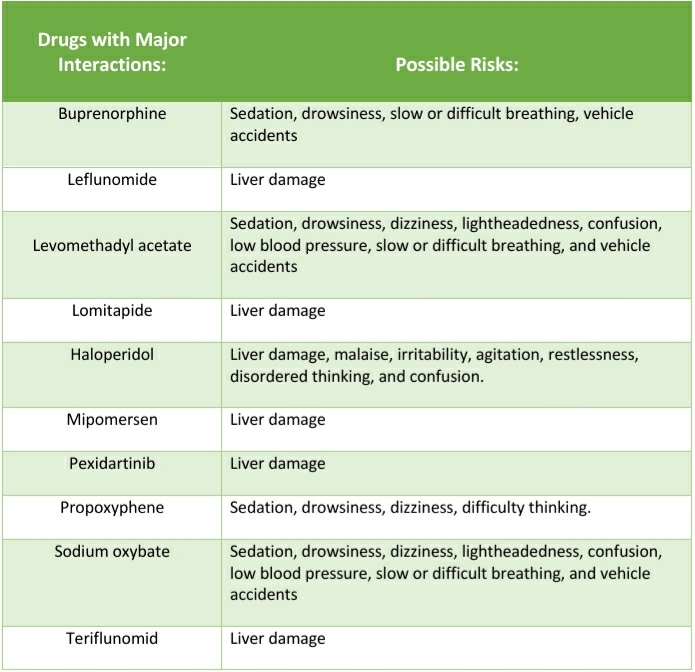
While we don’t yet know all the different drugs and supplements that cause interactions with CBD there are a few important ones to discuss. Ask your medical provider or pharmacist if you are taking any medications metabolized by the “cytochrome P450 3A and 2C enzymes”. CBD can change the ability of your liver to process those medications (Atalay, 2019). If you are taking any of the medications listed below please talk to your medical provider or pharmacist before starting CBD because they can cause serious interactions:
Conclusion and Considerations
CBD is a very unique chemical from the Cannabis sativa plant that can help you with pain. CBD lowers inflammation and changes how you feel and react to pain through multiple different mechanisms. More research and clinical trials will shed more light on the details of CBD use and until then there are many unknowns. Talk to your medical provider or pharmacist about any concerns you have and try CBD several different ways to find what works best for you.
If you can not use CBD due to liver problems or drug interactions do not worry! CBD is only one option for manipulating the endocannabinoid system to treat pain and inflammation. A variety of supplements, spices, and lifestyle changes have shown some ability to treat pain through similar mechanisms including:
Capsaicin – A desensitizer of TRPV1 receptors found in chili peppers. It is dissolved in creams and applied to the joints for arthritis pain (Anand, 2011).
Peppermint – A type of mint known for its cooling and anti-inflammatory properties. The menthol in peppermint activates TRPM8 which helps with certain types of pain (Liu, 2013).
Beta-Caryophyllene – A chemical found in a variety of spices including black pepper, cloves, hops, and oregano. It activates CB2 and PPARy receptors to lower inflammation and inflammatory pain (Cheng, 2014).
Palmitoylethanolamide and Oleoylethanolamide – These chemicals are known as fatty acid amides and they are found in a variety of foods. You can also purchase them as purified supplements. The fatty acid amides are involved in regulating the endocannabinoid system and have an affect on the TRPV receptors (Pillarisetti, 2009). They have shown some benefits in treating pain (Gabrielsson, 2016; Suardiaz, 2007).

Judd Harper is an independent contractor, entrepreneur, and proud parent. He studies multiple subjects including medicine, organic chemistry, pharmacology, botany, and mycology. He successfully uses Complimentary and Alternative Medicines (CAM’s) for his Crohn’s disease and advocates for health care reform and informed consent. He loves to spend time with his son, garden, listen to music, and learn new languages. He can be contacted at juddtharper@gmail.com with any questions or business solicitations.
References
- Alaverdashvili, M., & Laprairie, R. B. (2018, February). The Future of Type 1 Cannabinoid Receptor Allosteric Ligands. Retrieved July 10, 2020, from https://pubmed.ncbi.nlm.nih.gov/29355038/
- Anand, P., & Bley, K. (2011, October). Topical capsaicin for pain management: Therapeutic potential and mechanisms of action of the new high-concentration capsaicin 8% patch. Retrieved July 13, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3169333/
- Atalay, S., Jarocka-Karpowicz, I., & Skrzydlewska, E. (2019, December 25). Antioxidative and Anti-Inflammatory Properties of Cannabidiol. Retrieved July 11, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7023045/
- Bergamaschi, M. M., Queiroz, R. H., Zuwardi, A. W., & Crippa, J. A. (2011, September 1). Safety and Side Effects of Cannabidiol, a Cannabis Sativa Constituent. Retrieved July 07, 2020, from https://pubmed.ncbi.nlm.nih.gov/22129319/
- Bie, B., Wu, J., Foss, J. F., & Naguib, M. (2018, August). An overview of the cannabinoid type 2 receptor system and its therapeutic potential. Retrieved July 11, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6035094/
- Bruni, N., Della Pepa, C., Oliaro-Bosso, S., Pessione, E., Gastaldi, D., & Dosio, F. (2018, September 27). Cannabinoid Delivery Systems for Pain and Inflammation Treatment. Retrieved July 03, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6222489/
- Bushlin, I., Gupta, A., Stockton, S. D., Miller, L. K., & Devi, L. A. (2012). Dimerization with cannabinoid receptors allosterically modulates delta opioid receptor activity during neuropathic pain. Retrieved July 10, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3522681/
- Cheng, Y., Dong, Z., & Liu, S. (2014, August 26). β-Caryophyllene Ameliorates the Alzheimer-Like Phenotype in APP/PS1 Mice through CB2 Receptor Activation and the PPARγ Pathway. Retrieved July 13, 2020, from https://www.karger.com/Article/Abstract/362689
- Cherniakov, I., Izgelov, D., Domb, A. J., & Hoffman, A. (2017, July 20). The Effect of Pro NanoLipospheres (PNL) Formulation Containing Natural Absorption Enhancers on the Oral Bioavailability of delta-9-tetrahydrocannabinol (THC) and Cannabidiol (CBD) in a Rat Model. Retrieved July 02, 2020, from https://pubmed.ncbi.nlm.nih.gov/28736128/
- Consroe, P., Laguna, J., Allender, J., Snider, S., Stern, L., Sandyk, R., . . . Schram, K. (1991, November). Controlled Clinical Trial of Cannabidiol in Huntington’s Disease. Retrieved July 03, 2020, from https://pubmed.ncbi.nlm.nih.gov/1839644/
- Corroon, J., & Phillips, J. A. (2018, July 01). A Cross-Sectional Study of Cannabidiol Users. Retrieved July 07, 2020, from https://www.liebertpub.com/doi/full/10.1089/can.2018.0006
- Costa, B., Giagnoni, G., Franke, C., Trovato, A. E., & Colleoni, M. (2004, September). Vanilloid TRPV1 receptor mediates the antihyperalgesic effect of the nonpsychoactive cannabinoid, cannabidiol, in a rat model of acute inflammation. Retrieved July 13, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1575333/
- Craft, R. M., & Leitl, M. D. (2008, January 6). Gonadal Hormone Modulation of the Behavioral Effects of Delta9-tetrahydrocannabinol in Male and Female Rats. Retrieved July 01, 2020, from https://pubmed.ncbi.nlm.nih.gov/17905227/
- Craft, R. M., Marusich, J. A., & Wiley, J. L. (2013, March 19). Sex differences in cannabinoid pharmacology: A reflection of differences in the endocannabinoid system? Retrieved July 01, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3492530/
- Deliu, E., Sperow, M., Console-Bram, L., Carter, R. L., Tilley, D. G., Kalamarides, D. J., . . . Abood, M. E. (2015, August 01). The Lysophosphatidylinositol Receptor GPR55 Modulates Pain Perception in the Periaqueductal Gray. Retrieved July 11, 2020, from http://molpharm.aspetjournals.org/content/88/2/265
- Fattore, L., & Fratta, W. (2010, June). How important are sex differences in cannabinoid action? Retrieved July 04, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2931555/
- Gabrielsson, L., Mattsson, S., & Fowler, C. J. (2016, October). Palmitoylethanolamide for the treatment of pain: Pharmacokinetics, safety and efficacy. Retrieved July 13, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5094513/
- Godlewski, G., Wagner, J. A., & Kunos, G. (2009, September). Receptors for acylethanolamides-GPR55 and GPR119. Retrieved July 11, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2751869/
- Gregorio, D. D., McLaughlin, R. J., Posa, L., Ochoa-Sanchez, R., Enns, J., Lopez-Canul, M., . . . Gobbi, G. (2019, January). Cannabidiol Modulates Serotonergic Transmission and Reverses Both Allodynia and Anxiety-Like Behavior in a Model of Neuropathic Pain. Retrieved July 11, 2020, from https://pubmed.ncbi.nlm.nih.gov/30157131/
- Gunasekaran, N., Long, L. E., Dawson, B. L., Hansen, G. H., Richardson, D. P., Li, K. M., . . . McGregor, I. S. (2009, November). Reintoxication: The release of fat-stored delta(9)-tetrahydrocannabinol (THC) into blood is enhanced by food deprivation or ACTH exposure. Retrieved July 04, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2782342/?report=reader
- Hammell, D. C., Zhang, L. P., Ma, F., Abshire, S. M., McIlwrath, S. L., Stinchcomb, A. L., & Westlund, K. N. (2016, July 1). Transdermal cannabidiol reduces inflammation and pain-related behaviours in a rat model of arthritis. Retrieved July 02, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4851925/
- Hind, W., England, T. J., & O’Sullivan, S. E. (2015, October 24). Cannabidiol protects an in vitro model of the blood–brain barrier from oxygen‐glucose deprivation via PPARγ and 5‐HT1A receptors. Retrieved July 12, 2020, from https://bpspubs.onlinelibrary.wiley.com/doi/full/10.1111/bph.13368
- Holland, M. L., Lau, D. T., Allen, J. D., & Arnold, J. C. (2007, November). The multidrug transporter ABCG2 (BCRP) is inhibited by plant-derived cannabinoids. Retrieved July 04, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2190019/
- Huestis, M. A. (2007, August). Human cannabinoid pharmacokinetics. Retrieved July 04, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2689518/
- Ibeas Bih, C., Chen, T., Nunn, A. V., Bazelot, M., Dallas, M., & Whalley, B. J. (2015, October). Molecular Targets of Cannabidiol in Neurological Disorders. Retrieved July 12, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4604182/
- Iffland, K., & Grotenhermen, F. (2017, June 1). An Update on Safety and Side Effects of Cannabidiol: A Review of Clinical Data and Relevant Animal Studies. Retrieved July 02, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5569602/
- Izgelov, D., Domb, A. J., & Hoffman, A. (2020, May 30). The Effect of Piperine on Oral Absorption of Cannabidiol Following Acute vs. Chronic Administration. Retrieved July 01, 2020, from https://pubmed.ncbi.nlm.nih.gov/32198013/
- Jean-Gilles, L., Braitch, M., Latif, M. L., Aram, J., Fahey, A. J., Edwards, L. J., . . . Constantinescu, C. S. (2015, May). Effects of pro-inflammatory cytokines on cannabinoid CB1 and CB2 receptors in immune cells. Retrieved July 11, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4669958/?report=reader
- Jesus, C. H., Redivo, D. B., Gasparin, A. T., Sotomaior, B. B., Carvalho, M. C., Genaro, K., . . . Cunha, J. M. (2018, September 4). Cannabidiol attenuates mechanical allodynia in streptozotocin-induced diabetic rats via serotonergic system activation through 5-HT1A receptors. Retrieved July 11, 2020, from https://www.sciencedirect.com/science/article/abs/pii/S0006899319301532
- Klinger-Gratz, P. P., Ralvenius, W. T., Neumann, E., Kato, A., Nyilas, R., Lele, Z., . . . Zeilhofer, H. U. (2018, January 10). Acetaminophen Relieves Inflammatory Pain Through CB 1 Cannabinoid Receptors in the Rostral Ventromedial Medulla. Retrieved July 09, 2020, from https://pubmed.ncbi.nlm.nih.gov/29167401/
- Laprairie, R. B., Bagher, A. M., Kelly, M. E., & Denovan-Wright, E. M. (2015, October 13). Cannabidiol Is a Negative Allosteric Modulator of the Cannabinoid CB1 Receptor. Retrieved July 10, 2020, from https://pubmed.ncbi.nlm.nih.gov/26218440/
- Liu, B., Fan, L., Balakrishna, S., Sui, A., Morris, J., & Jordt, S. (2013, October). TRPM8 is the principal mediator of menthol-induced analgesia of acute and inflammatory pain. Retrieved July 13, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3778045/
- Manini, A. F., Yiannoulos, G., Bergamaschi, M. M., Hernandez, S., Olmedo, R., Barnes, A. J., . . . Hurd, Y. L. (2015). Safety and pharmacokinetics of oral cannabidiol when administered concomitantly with intravenous fentanyl in humans. Retrieved July 06, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4449284/
- Manzanares, J., Julian, M., & Carrascosa, A. (2006, July). Role of the cannabinoid system in pain control and therapeutic implications for the management of acute and chronic pain episodes. Retrieved July 10, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2430692/
- McPartland, J. M., Duncan, M., Di Marzo, V., & Pertwee, R. G. (2015, February). Are cannabidiol and Δ(9) -tetrahydrocannabivarin negative modulators of the endocannabinoid system? A systematic review. Retrieved July 12, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4301686/?report=reader
- Mecha, M., Feliú, A., Iñigo, P. M., Mestre, L., Carrillo-Salinas, F. J., & Guaza, C. (2013, July 11). Cannabidiol provides long-lasting protection against the deleterious effects of inflammation in a viral model of multiple sclerosis: A role for A2A receptors. Retrieved July 12, 2020, from https://www.sciencedirect.com/science/article/pii/S0969996113001939
- Meyer, P., Langos, M., & Brenneisen, R. (2018, June 12). Human Pharmacokinetics and Adverse Effects of Pulmonary and Intravenous THC-CBD Formulations. Retrieved July 03, 2020, from https://www.karger.com/article/fulltext/489034
- Millar, S. A., Stone, N. L., Bellman, Z. D., Yates, A. S., England, T. J., & O’Sullivan, S. E. (2019, September). A systematic review of cannabidiol dosing in clinical populations. Retrieved June 28, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6710502/
- Millar, S. A., Stone, N. L., Yates, A. S., & O’Sullivan, S. E. (2018, November 26). A Systematic Review on the Pharmacokinetics of Cannabidiol in Humans. Retrieved July 01, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6275223/
- Muller, C., Morales, P., & Reggio, P. (2019, January 15). Cannabinoid Ligands Targeting TRP Channels. Retrieved July 13, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6340993/
- Nahler, G., & Jones, T. M. (2018, April 30). Pure Cannabidiol versus Cannabidiol-Containing Extracts: Distinctly Different Multi-Target Modulators. Retrieved July 12, 2020, from http://www.heraldopenaccess.us/openaccess/pure-cannabidiol-versus-cannabidiol-containing-extracts-distinctly-different-multi-target-modulators
- O’Sullivan, S. E. (2016, June). An update on PPAR activation by cannabinoids. Retrieved July 12, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4882496/?report=reader
- Palazzo, E., Luongo, L., Novellis, V., Rossi, F., & Maione, S. (2010, August 16). The Role of Cannabinoid Receptors in the Descending Modulation of Pain. Retrieved July 10, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4033943/
- Petrocellis, L. D., Ligresti, A., Moriello, A. S., Allarà, M., Bisogno, T., Petrosino, S., . . . Marzo, V. D. (2011, August). Effects of cannabinoids and cannabinoid-enriched Cannabis extracts on TRP channels and endocannabinoid metabolic enzymes. Retrieved July 13, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3165957/?report=reader
- Petrocellis, L. D., Vellani, V., Schiano-Moriello, A., Marini, P., Magherini, P. C., Orlando, P., & Marzo, V. D. (2008, June). Plant-derived Cannabinoids Modulate the Activity of Transient Receptor Potential Channels of Ankyrin type-1 and Melastatin type-8. Retrieved July 13, 2020, from https://pubmed.ncbi.nlm.nih.gov/18354058/
- Petrosino, S., Verde, R., Vaia, M., Allarà, M., Iuvone, T., & Marzo, V. D. (2018, June). Anti-inflammatory Properties of Cannabidiol, a Nonpsychotropic Cannabinoid, in Experimental Allergic Contact Dermatitis. Retrieved July 11, 2020, from https://pubmed.ncbi.nlm.nih.gov/29632236/
- Pillarisetti, S., Alexander, C. W., & Khanna, I. (2009, December). Pain and Beyond: Fatty Acid Amides and Fatty Acid Amide Hydrolase Inhibitors in Cardiovascular and Metabolic Diseases. Retrieved July 13, 2020, from https://pubmed.ncbi.nlm.nih.gov/19716430/
- Quirion, B., Bergeron, F., Blais, V., & Gendron, L. (2020, March 13). The Delta-Opioid Receptor; a Target for the Treatment of Pain. Retrieved July 10, 2020, from https://www.frontiersin.org/articles/10.3389/fnmol.2020.00052/full
- Russo, E. B., Burnett, A., Hall, B., & Parker, K. K. (2005, August). Agonistic Properties of Cannabidiol at 5-HT1a Receptors. Retrieved July 11, 2020, from https://pubmed.ncbi.nlm.nih.gov/16258853/
- Stančić, A., Jandl, K., Hasenöhrl, C., Reichmann, F., Marsche, G., Schuligoi, R., . . . Schicho, R. (2015, July 30). The GPR55 antagonist CID16020046 protects against intestinal inflammation. Retrieved July 11, 2020, from https://onlinelibrary.wiley.com/doi/abs/10.1111/nmo.12639
- Staton, P. C., Hatcher, J. P., Walker, D. J., Morrison, A. D., Shapland, E. M., Hughes, J. P., . . . Chessell, I. P. (2008, May 27). The putative cannabinoid receptor GPR55 plays a role in mechanical hyperalgesia associated with inflammatory and neuropathic pain. Retrieved July 11, 2020, from https://www.sciencedirect.com/science/article/abs/pii/S0304395908001942
- Suardiaz, M., Estivill-Torrús, G., Goicoechea, C., Bilbao, A., & Fonseca, F. R. (2007, December 15). Analgesic Properties of Oleoylethanolamide (OEA) in Visceral and Inflammatory Pain. Retrieved July 13, 2020, from https://pubmed.ncbi.nlm.nih.gov/17449181/
- Tham, M., Yilmaz, O., Alaverdashvili, M., Kelly, M., Denovan‐Wright, E., & Laprairie, R. (2018, August 10). Allosteric and orthosteric pharmacology of cannabidiol and cannabidiol‐dimethylheptyl at the type 1 and type 2 cannabinoid receptors. Retrieved July 11, 2020, from https://bpspubs.onlinelibrary.wiley.com/doi/full/10.1111/bph.14440
- Ward, S. J., McAllister, S. D., Kawamura, R., Murase, R., Neelakantan, H., & Walker, E. A. (2014, January 13). Cannabidiol inhibits paclitaxel‐induced neuropathic pain through 5‐HT1A receptors without diminishing nervous system function or chemotherapy efficacy. Retrieved July 11, 2020, from https://bpspubs.onlinelibrary.wiley.com/doi/full/10.1111/bph.12439
- Weiss, F., & Gonzalez-Cuevas, G. (2018, September 25). Unique treatment potential of cannabidiol for the prevention of relapse to drug use. Retrieved July 08, 2020, from https://www.nature.com/articles/s41386-018-0218-2
- Xu, D. H., Cullen, B. D., Tang, M., & Vang, Y. (2020, May 21). The Effectiveness of Topical Cannabidiol Oil in Symptomatic Relief of Peripheral Neuropathy of the Lower Extremities. Retrieved July 02, 2020, from https://pubmed.ncbi.nlm.nih.gov/31793418/
- Zgair, A., Wong, J., Lee, J., Mistry, J., Sivak, O., Wasan, K. M., . . . Gershkovich, P. (2016, August 15). Dietary fats and pharmaceutical lipid excipients increase systemic exposure to orally administered cannabis and cannabis-based medicines. Retrieved July 02, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5009397/